TMJ dysfunction explained: what’s actually going on?
TMJ dysfunction is a term that gets used a lot, often loosely. Some people are told they “have TMJ” without much explanation. Others are left wondering whether jaw pain, clicking, headaches or facial tension are connected at all.
To make sense of it, it helps to start with what the TMJ actually is.
What is the TMJ?
TMJ stands for temporomandibular joint. You have one on each side of your face, just in front of the ears, where the lower jaw meets the skull. These joints allow you to open and close your mouth, chew, speak and yawn.
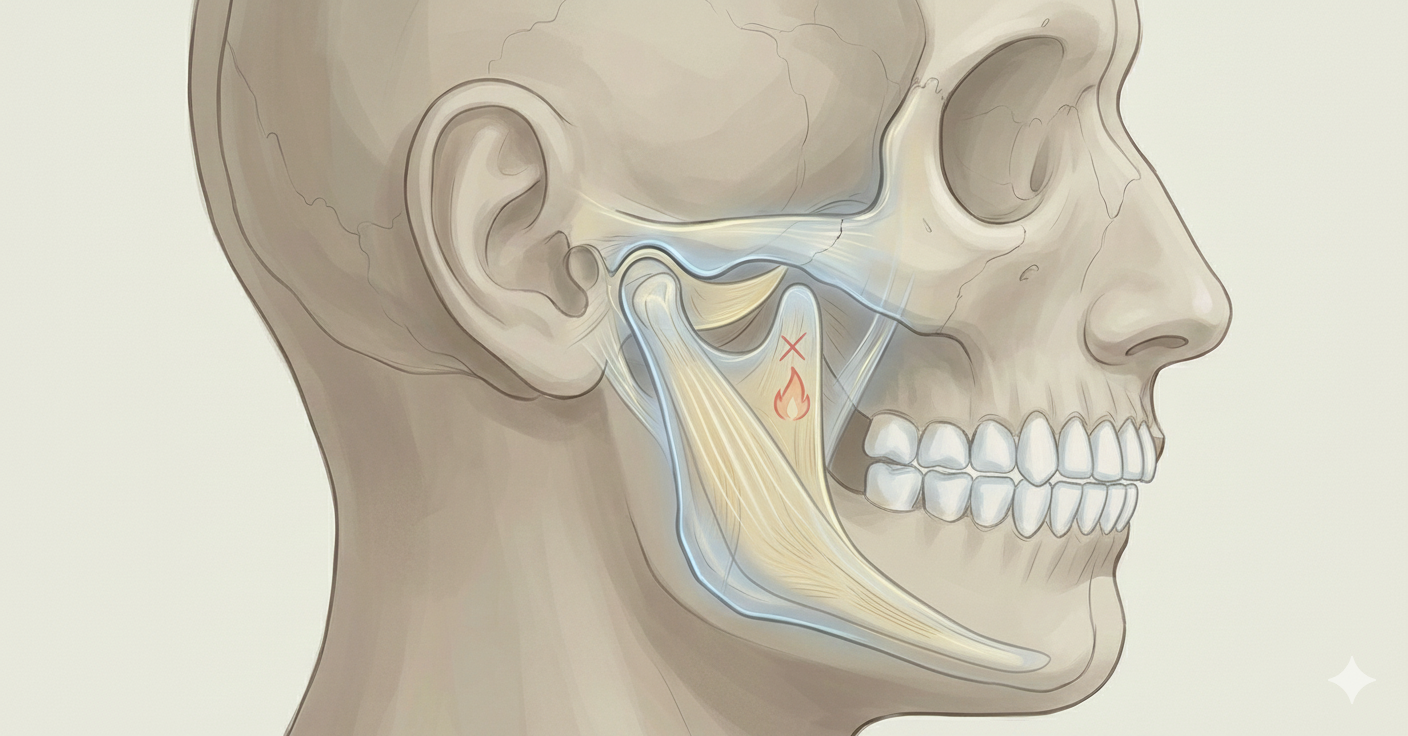
The TMJ is a complex joint. It doesn’t simply hinge open and closed. It also glides forward and back, and it relies on a coordinated relationship between:
the joint surfaces
a small cartilage disc within the joint
surrounding muscles
the nervous system
Because of this complexity, symptoms can arise from several different structures, not just the joint itself.
What does “TMJ dysfunction” actually mean?
TMJ dysfunction is an umbrella term. It doesn’t describe a single diagnosis or one specific problem.
It’s generally used when pain, restriction, clicking, locking or altered movement occurs in or around the jaw joint, and when these symptoms can’t be explained by a simple fracture or acute injury.
TMJ-related symptoms can include:
jaw pain or aching
clicking, popping or grinding noises
difficulty opening the mouth fully
deviation of the jaw when opening
facial pain
headaches
neck pain or upper shoulder tension
ear-related symptoms such as fullness or ringing
Not everyone experiences all of these. Some people have significant noise with little pain. Others have pain without any obvious clicking.
Is clicking always a problem?
No. Joint noise on its own is not necessarily a sign of dysfunction.
Clicking often relates to the movement of the disc within the joint. In some cases, the disc doesn’t move as smoothly as it should and briefly catches during opening or closing. This can produce a click.
Importantly:
many people have clicking without pain
not all clicking requires treatment
the presence of noise alone does not predict damage
What matters more is whether the clicking is accompanied by pain, locking, progressive restriction, or changes in function.
It’s also worth noting that not all disc-related issues involve clicking.
In some cases, the disc within the temporomandibular joint becomes displaced and does not return to its usual position during movement. This is often referred to as disc displacement without reduction. When this happens, the jaw may stop clicking altogether, but instead feel tight, restricted or persistently sore.
Because the disc plays a role in cushioning and load distribution within the joint, reduced disc function can mean the joint itself has less protection. Over time, this may contribute to irritation or degenerative changes within the joint, although this is not inevitable and varies greatly between individuals.
Importantly, this means that a jaw which feels tense, stiff or painful without any clicking can still be experiencing disc-related dysfunction. Equally, symptoms are often influenced by muscular guarding and nervous system sensitivity, not just joint structure alone.
Muscles vs joints: an important distinction
One of the most common misunderstandings around TMJ issues is assuming the joint itself is always the primary problem.
In practice, a large proportion of TMJ-related pain is muscular, not structural.
Muscles that commonly contribute include those responsible for:
closing the jaw
stabilising the head and neck
maintaining posture during prolonged sitting or screen use
When these muscles are overactive, fatigued or sensitised, they can refer pain into the jaw, face, head and neck. This can mimic joint pain very convincingly.
This is one reason why imaging alone often fails to explain symptoms. Scans may show age-related changes or disc variations that are not actually driving the pain.
The role of the nervous system
The jaw is particularly sensitive to nervous system input. Stress, sustained concentration and emotional load can all influence muscle tone around the TMJ.
In people under prolonged stress, the nervous system may maintain a higher baseline level of activation. Muscles around the jaw and neck can remain subtly switched on, even at rest. Over time, this can contribute to pain, stiffness and reduced tolerance to normal movement.
This does not mean symptoms are “all in your head”. It means that pain is being influenced by how the nervous system is regulating muscle activity and threat perception.
Why TMJ symptoms often overlap with neck pain and headaches
The jaw does not function in isolation. It is closely linked to the upper cervical spine and surrounding structures.
Changes in jaw movement or muscle tone can influence:
head position
neck muscle activity
load through the upper cervical joints
Similarly, neck posture and upper body tension can alter how the jaw moves and how much effort is required to stabilise it.
This two-way relationship is why effective assessment looks beyond the jaw itself.
When is TMJ treatment appropriate?
Hands-on treatment can be appropriate when:
pain is persistent or recurrent
jaw symptoms are accompanied by neck pain or headaches
clenching or muscle tension is a contributing factor
movement feels restricted or uncomfortable
symptoms fluctuate with stress or workload
The aim is not to force change at the joint, but to address the surrounding tissues, movement patterns and nervous system input that may be maintaining symptoms.
A careful, individualised approach
TMJ-related issues benefit from a measured, individual approach. There is no single technique or exercise that works for everyone.
Effective management often involves:
a clear assessment of jaw, neck and upper body movement
addressing muscle tone and tissue sensitivity
improving awareness of jaw position and load
supporting the nervous system to reduce unnecessary tension
For some people, this also sits alongside dental input, particularly where night-time grinding, splint use or bite-related factors are involved.
If you’re unsure what’s driving your symptoms
If you’ve been told you have TMJ dysfunction but haven’t been given a clear explanation, or if your symptoms don’t quite fit the label you’ve been given, that uncertainty alone can be frustrating.
Understanding what’s actually going on is often the first step towards improvement.
If you’d like to explore this further, you can read more about my Head, Jaw & Neck therapy and how this approach is used to assess and support TMJ-related pain.